Chromomycosis, or Chronic subcutaneous mycosis, is a severe fungal infectious disease that infects the skin’s subcutaneous tissue. A diverse group of dematiaceous or black fungi cause chromomycosis. Dematiaceous fungi are the heterogeneous fungal group, which usually form lesions or abscess in the subcutaneous tissue.
Interaction of host tissue with the fungus shows a non-specific kind of response. Macrophages and neutrophils play a significant role to create an immunological response against this disease. Chromomycosis is sometimes interchangeable with the terms chromoblastomycosis or phaeohyphomycosis.
Dematiaceous fungi include Fonsecaea pedrosoi, Phialophora verrucosa, Cladosporium carrionii etc., that may enter the subcutaneous tissue through the skin surface. In this context, you would get to know the causative agent of chromomycosis disease along with its distribution, risk factors, clinical features, diagnosis and treatment.
Content: Chromomycosis
Causative Agent of Chromomycosis
Dematiaceous fungi are the aetiological agents, which belong to the phylum “Ascomycota” and order “Chaetothyriales”. Dematiaceous fungi undergo cell division meristematically, not through budding. They cause septation that infects the subcutaneous tissue.
The transmission of the fungus generally results via autoinoculation, i.e. through scratching the infected site to the other parts. A group of dematiaceous fungi are ubiquitous in soil, plants and plant debris. Thus, barefoot agriculture workers and woodcutters are highly affected by this disease.
Distribution
Chromomycosis mainly occurs in subtropical and tropical regions like Asia and America. Many cases resulted in Mexico, Cuba etc. and outside the American continents (first case in 1927). In Africa, most cases were reported in Madagascar and South Africa. In Asia, chromomycosis is more prevalent in countries like Japan, Sri Lanka, India etc. Thus, the distribution of chromomycosis is worldwide.
Risk Factors
Chromomycosis is more prevalent in males having an age limit between 30 and 50 years and those engaged in agricultural activities. A person with HLA-A 29 antigen is ten times more susceptible to this disease.
- In males: Chromomycosis prevalently affects the upper limbs, buttocks and lower limbs.
- In females: Chromomycosis prevalently affects the upper limbs, neck, face and lower limbs.
The occurrence of the disease is more common to the site of lower limbs, as it is in direct contact with the soil, plants, debris which might carry the fungal spores.
Clinical Symptoms
The most common feature of chromomycosis is the appearance of sclerotic lesions on the skin. The disease mainly affects the upper limbs, lower limbs and buttock area.
Initial stage: Small red or grey bump appears during the initial stage, and eventually warty dry nodule appears called “Primary lesions”. The formation of lesions is confined to the subcutaneous tissues of the feet and lower legs.
The size and shape of the warty lesions vary from person to person. The disease progresses very slowly and may take up to 10 years from the infection to the diagnosis. Based on the morphological features, a lesion can be of five types:
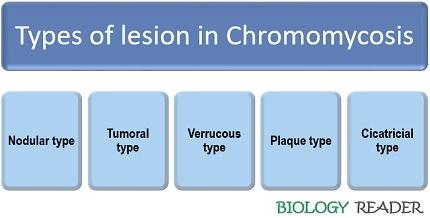
Nodular type
It occurs most frequently. Nodular type lesions are characterized by the following features:
- Colour of lesion: Pale pink in colour.
- The appearance of lesion: Soft lesion with slightly raised papules.
- The surface of lesion: Smooth, papillary and scaly.
- Further, many nodules transform into tumoral lesion.
Tumoral type
It is characterized by the following features:
- The appearance of lesion: Large and protruding papules.
- The surface of the lesion: Lobulated and covered with dirty grey epidermal remains.
- The shape of the lesion: Resembles the shape of Cauliflower.
- Size of lesion: Lesion forms tumoral masses that gradually grow in size.
Verrucous type
The appearance of hyperkeratotic lesions shows a sign of having verrucous chromomycosis that usually occurs in the upper or lower limbs. It most frequently affects the edges of the feet.
Plaque type
It occurs very frequently with various shapes and sizes. Plaque-type lesions are reddish to violet in colour with a scaly surface.
Cicatricial type
It results in annular and arched lesions in the substantial areas of the body.
Complications: The complications of chromomycosis involve secondary infections and ulcerations. In severe cases, it leads to lymphoedema and ankylosis. Chromomycosis results in swelling of limbs, which leads to elephantitis. The lesions become carcinogenic that results in the development of squamous cell carcinoma. Fonsecaea pedrosoi also cause brain abscesses.
Based on the severity, chromomycosis is classified into three types:
- Mild form: The condition is mild if a single nodule forms having a diameter greater than 5 cm.
- Moderate form: The condition is moderate if single or multiple nodules of tumoral, verrucous or plaque-type forms with a diameter greater than 15 cm.
- Severe form: A condition is severe if the diameter of the lesion exceeds by covering the extensive skin areas.
Diagnosis
Chromomycosis diagnosis requires thick-walled, sclerotic muriform cells or medlar bodies from the skin scraping.
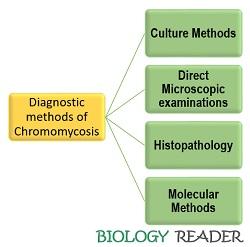
Culture method: You need to culture the sample of the infected site in selective media like Sabouraud agar media (SDA) supplemented with cycloheximide. On standard media, chromomycosis can be characterized by the slow growth of black colonies. For further assessment of the disease, the slide culture method is usually employed to determine the microscopic features.
Direct examination: We could examine the presence of sclerotic medlar bodies by preparing potassium hydroxide mounts. It results in dark golden brown, sub-globose, multicellular, planate and dividing yeast cells of medlar bodies.
Other techniques: Techniques like biopsy and molecular methods confirm the diagnosis. Duplex PCR of ribosomal DNA diagnoses Fonsecaea sp. and oligonucleotide primer diagnoses the presence of C. carrionii.
Treatment of Chromomycosis
Its treatment involves the following chemical and physical methods.
Chemical Methods
It includes treatment of chromomycosis with antifungal agents like:
- Itraconazole: Based on the severity of the disease, a daily dose of Itraconazole with 200-400 mg is generally recommended. In mild cases, a disease recovers within 6-12 months. But in severe cases, it takes several months. Itraconazole behaves as a “Fungistatic agent”, so there may be a chance of relapsing the disease.
- Terbinafine: It is an antifungal agent recommended with a daily dose of 500-1000 mg.
- Posaconazole: It is effective with a dose of 800 mg/day.
- 5-Flourocytosine: It is not effective but usually recommended with a dose of 100-150mg/kg/day in four doses for 6-12 months.
Physical Methods
It includes surgical excision, cryosurgery, thermotherapy and laser vaporisation.
- Surgical excision: It only treats the primary lesions limited in number, not effective in treating secondary lesions.
- Cryosurgery: It treats chromomycosis by using liquid nitrogen in combination with Itraconazole therapy. The cryosurgery method destroys the fungus within 1-2 weeks from the site of the lesion.
- Thermotherapy: It uses pocket warmers, which are allowed to place on the lesion site for 24 hours. Thermotherapy is effective in conjugation with antifungal chemotherapy.
- Laser vaporisation: This method, in combination with thermotherapy, can successfully excise the sclerotic nodules. The laser vaporisation method treats the buttock lesions.
Conclusion
Chromomycosis or chromoblastomycosis is a subcutaneous infection that primarily results in the formation of dark coloured sclerotic cells over the skin surface. Its treatment becomes necessary because untreated chromoblastomycosis may lead to squamous cell carcinomas (a skin cancer type).